
For best results make sure background graphics are enabled.
| Table of contents |
| What is an upper respiratory tract infection? |
What is an upper respiratory tract infection?
Upper respiratory tract infections (URTIs) are extremely common — that's why they're often called the "common cold". They're so common in fact that it's normal for children under five years old to have as many as 12 URTIs in one year.
What is an upper respiratory tract infection?
Upper respiratory tract infections (URTIs) are extremely common — that's why they're often called the "common cold". They're so common in fact that it's normal for children under five years old to have as many as 12 URTIs in one year. Typical URTI symptoms include: blocked or runny nose (mucous),cough, fever, red eyes, reduced appetite, less energy than normal and sore throat.

Symptoms
URTIs cause symptoms in the nose, throat and sinuses. Typical URTI symptoms include:
- blocked or runny nose (mucous)
- cough
- fever
- red eyes
- reduced appetite
- less energy than normal
Why did my child get sick?
It's common for younger children to get URTIs from daycare or other siblings at home. The good news is that the each time your child has a URTI, their immunity (ability to fight off viruses) will improve.
How are URTIs spread?
A URTI can be passed from person to person through the air or on commonly touched surfaces. For example, your child could pick up a URTI if:
- someone coughed or sneezed the virus into the air and they breathed it in
- they touched a hard surface (like a toy) with the virus on it, and then touched their mouth, nose or eyes.
Did you know? URTIs are not caused by cold air or drafts! Because these viruses circulate more commonly in the colder months, URTIs just happen to occur more during the fall and winter.
Helping your child or youth feel better at home
Most coughs, earaches, sinus congestion and sore throats get better at home without antibiotics. Most of the symptoms will improve in 7 to 10 days. Remember that a cough can last up to three weeks.
Congestion
URTIs usually start with clear mucous from the nose. This mucous might get thicker or become yellow/green in colour. This is normal and can last for a few days, Your child might have a hard time sleeping or feeding because their nose is "stuffed up". Saline (salt water) drops can help loosen mucous in the nose when your child is congested. Hydrasense® and Nosefrida® are brands that make nasal aspirators ("snot suckers"). To use, place two to three drops of saline in each nostril, especially before feeding or sleeping and use a nasal aspirator ("snot sucker") to remove mucous from the nostrils after using saline drops.
Raise your child's head: Raising the head of the bed to about 30 degrees will help your child to breathe easier so they can get some sleep. Use a wedge under the mattress for children under the age of 18 months (never leave your infant unsupervised asleep in a car-seat or swing). For older children, either a wedge or an extra pillow may help.
Cough
The cough is often the last symptom to go away. This is because your child's airway needs time to heal from the virus. Your child may continue to cough up to three weeks after the other symptoms have settled. DO NOT give cough and cold medicines to children less than six years old. These medications can cause unwanted side effects, such as drowsiness, dizziness, trouble falling asleep or rapid heart rate. Using these medications do not make the illness go away faster.
If your child is old enough, gargling warm salty water, or sucking on a throat lozenge can give relief. Undiluted honey (not in water or tea) has been shown to improve cough and sore throat for children older than one year. Use one teaspoon before bed and during bouts of coughing at night. Also, try to keep your home smoke free.
Sore throat and poor appetite
During a URTI you will notice a drop in your child’s appetite. It is important to make sure your child is drinking lots of fluids that have calories (like milk, juice or Pedialyte®). Popsicles are helpful if children are reluctant to drink. Drinking fluids is more important than eating during the period of illness. if the pain persists, you should treat their throat pain with ibuprofen or acetaminophen using our dosing guide.
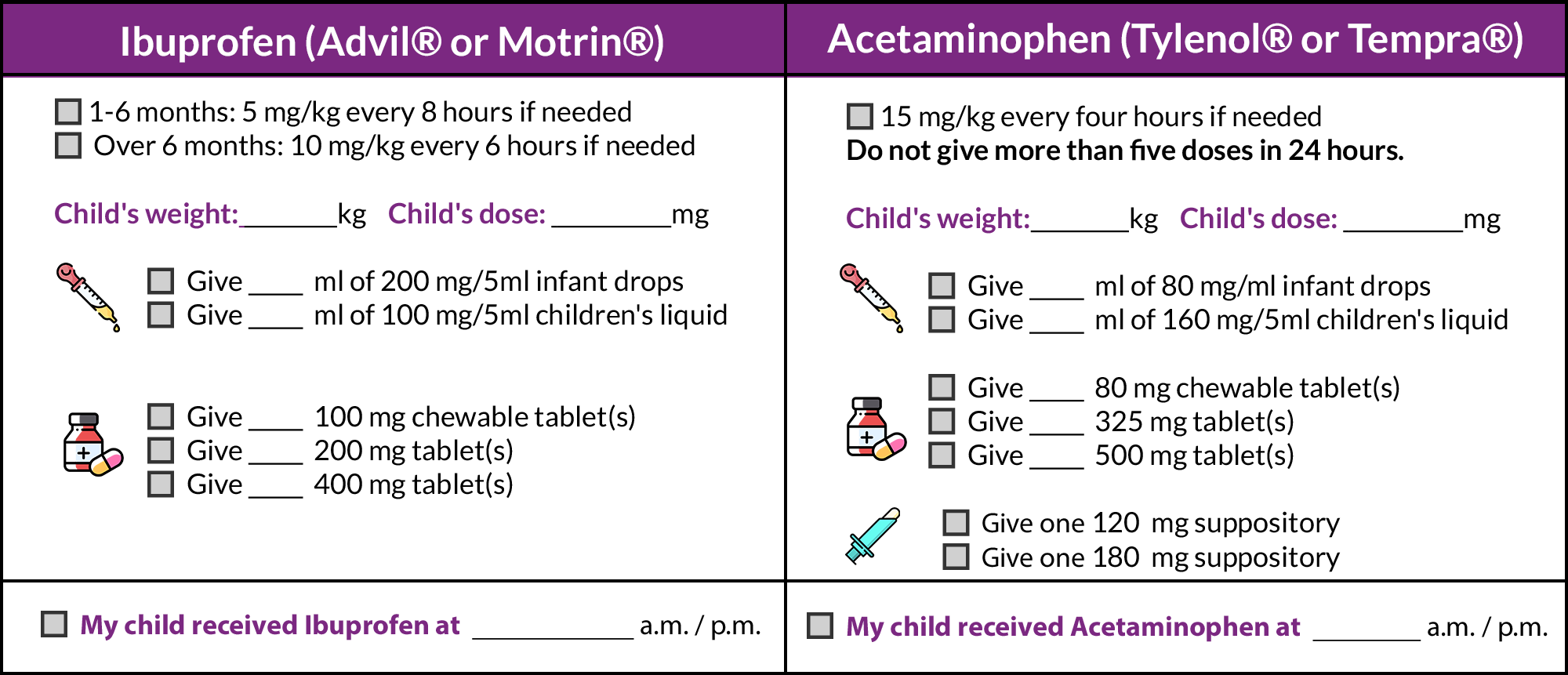
Fever medicines
Ibuprofen and acetaminophen can make your child more comfortable by bringing down the fever a little. Most children will not need to have both of these medications.
When your child has a fever:
- Try ibuprofen first, as it works better for most children. Use acetaminophen instead of ibuprofen if your child has a fever due to chicken pox.
- Try acetaminophen if your child does not improve one hour after taking ibuprofen
- Do not use Aspirin® (ASA).
How much should you give?
Medicines for fever and pain come in different concentrations (the number of mg of medicine in each mL, tablet or suppository). Check the concentration on the bottle, and read the package directions carefully. Make sure that you give the dose based on your child’s weight, not age.
When to see your family doctor
- the fever lasts more than four days
- your child isn't managing to drink enough fluids
- your child develops a new fever or has obvious ear pain
- their cough lasts more than 2-3 weeks
You know your child best. CHEO's ED is always here for you. Visit the ED if your child or youth:
- is under three months and has a fever
- is very irritable or sleepy and doesn't improve with medicine
- has difficulty breathing
- has signs of dehydration (dry mouth, not peeing at least every eight hours)
- has a headache or sore neck that doesn't go away with fever or pain medicine
- Hydrasense and Nose frieda are brands that make nasal aspirators ("snot sucker")




