
CHEO leads the way in tackling one of the most complex and critical areas of pediatric health care: eating disorders, with clinicians and researchers pioneering innovative approaches that are not only improving care at CHEO but also shaping health systems across Canada and beyond.
The COVID-19 pandemic brought the social and economic cost of eating disorders into the spotlight as a national study led by the CHEO Research Institute showed a significant increase of children and youth who visited the emergency department or were admitted to hospital with eating disorders.
The response at CHEO has involved many expert clinicians to improve the care when kids arrive at hospital, as well as long before they require hospital-based treatment.
Dr. Nicole Obeid, an applied developmental psychologist who is also the Scientist and Lead of the Eating Disorder Research Lab at the CHEO Research Institute, has prided her work on early detection and treatment.
Obeid said early intervention can significantly improve treatment response and outcomes, but the Canadian health-care system is not currently equipped to deliver that care.
“There are so many young people who struggle long before they develop a severe eating disorder,” she said, adding that 90 per cent of eating disorders begin before the age of 25.
Once someone shows initial signs of an eating disorder — such as preoccupations about weight and food, before the onset of full illness —it is important to detect it within the first three years, evidence shows, because early detection can limit severe impacts to one’s mental and physical health.
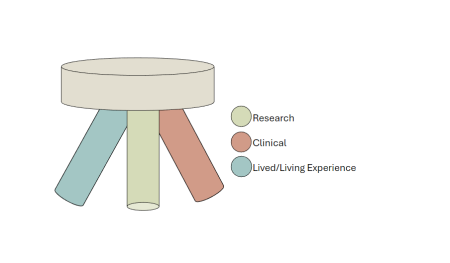
That inspired Obeid to help launch and lead the FREEDCan network, which adopts an evidence-based model started in the U.K. that combines research, clinical and lived experience. The model focuses on widespread screening to connect youth to health services as they manage early-stage eating disorders.
Obeid said studies still have not captured the complete picture of eating disorder prevalence, but clinicians at CHEO’s Eating Disorders Program continue to see significant demand for care.
They work to ensure every child and youth has the most effective treatment for their specific diagnosis, but options remain limited.
Those challenges inspired an innovative new model called the CHEO Eating Disorder Partial Hospitalization Program, the first of its kind in Canada. This program offers intensive, individualized care to children and youth with moderate to severe eating disorders— seven days a week, 12 hours a day — while allowing the patient to return home in the evening.
Since August 2022, the program has delivered care to 170 kids to help prevent, reduce, and shorten hospital stays. Less time in hospital helps preserve the psychosocial development of children and youth, said Dr. Leanna Isserlin, Chief of CHEO’s Department of Psychiatry and Medical Co-Director of the Eating Disorders Program.
 The partial hospitalization program can help anywhere from 12 to 15 patients each day, and Isserlin said the team has been able to add more clinicians to help treat kids faster.
The partial hospitalization program can help anywhere from 12 to 15 patients each day, and Isserlin said the team has been able to add more clinicians to help treat kids faster.
In April 2025, Isserlin and Dr. Elizabeth Quon, clinical psychologist and Clinical Lead of the Eating Disorders Program, were among team members who shared details about the program with an audience of Canadian pediatric health leaders at the Children's Healthcare Canada conference.
They believe the program’s innovative thinking, collaboration and growth can be applied to many other areas of pediatric health care as teams look for creative ways to fill care gaps.
Obeid’s FREEDCan work, while still in its infancy, has also inspired partnerships with eating disorders researchers in Australia, as well as the U.K.
As we mark Children's Mental Health Week and National Child and Youth Mental Health Day, CHEO’s leadership in the research and care of eating disorders aims to give every child and youth the best life through patient- and family-centred care, prioritizing early intervention and customizing care for every patient.





