Virtual Family-Centred Rounds (vFCR) Toolkit: An Implementation Guide for health-care leaders and providers
Looking for general information on virtual family-centred rounds at CHEO? Visit our family-centred rounds webpage here!
This toolkit was developed for health-care leaders and providers, by a multidisciplinary team of health-care professionals and researchers at CHEO. Its purpose is to sustain the use of virtual family-centred rounds at CHEO (when appropriate) and support the implementation of virtual family-centred rounds in other health-care organizations.
Why this Toolkit |
|
Given our experience and success with virtual family-centred rounds at CHEO, we wanted to develop a toolkit to support implementation beyond our walls, by sharing our process and learnings with you! In 2021 we received a grant funding to conduct an evaluation of our vFCR process and associated technology. Preliminary results are in, confirming feasibility and satisfaction with vFCR, but also highlighting the need for additional training and skill development to maximize efficiency and quality of care. Learn more about virtual care at CHEO including virtual family-centred rounds |
What is in this Toolkit |
|
In the Toolkit you'll find information and resources to help you bring virtual family-centred rounds to your own organization, including:
|
Who is this Toolkit for |
|
This toolkit is for hospital leaders, health-care providers and clinical educators working in inpatient areas. The content will be applicable and easily understood by all stakeholders involved in virtual family-centred rounds. For information on virtual family-centred rounds for patients, families, and caregivers, visit our family-centred rounds page. |
How to navigate this Toolkit |
|
For staff training
|
Overview of the vFCR process and roles
- The Unit clerk is responsible for creating and posting the rounding schedule and starting the virtual rounds videoconference for nurses and patients/caregivers
- The Care Facilitator or Charge Nurse is responsible for enabling and supporting nurse participation in rounds
- Nurses will prioritize rounds according to the rounding schedule and inform the Unit clerk, Charge Nurse, or Care Facilitator if they are unable to attend due to conflicting patient care needs.
- Physician Teams (i.e. attending physician and team) will commit to starting on time, adhering the rounding schedule, having focused rounding discussions and coordinating with other inpatient units as needed.
- Healthcare Professionals (including pharmacists, allied health care providers and consulting physicians) may join rounds for the patients they follow as appropriate
Family-Centred Rounds Standard Content |
||||||||||||||||||||
|
Training Material for Multidisciplinary Care Team Members
Training for Nursing Staff and Students
Find more information on roles and responsibilities for nursing staff and nursing students |
|
As the patient’s nurse, you are an essential member of the multidisciplinary care team and your presence on daily rounds is vitally important. You should prioritize daily rounds and inform the care team if you are unable to attend due to competing patient care demands. Your responsibilities in virtual family-centred rounds include:
The care facilitator (and/or charge nurse) is responsible for supporting nurse participation in rounds and ensuring timely transitions between nurses. This may include covering patient care or coordinating schedule adjustment with the unit clerk if a nurse cannot attend rounds as scheduled. The following resources provide more information on these responsibilities and detailed instructions for nursing: |

Training for Unit Clerks
Find more information on the roles and responsibilities for unit clerks |
|
As the unit clerk, you have the important responsibility of setting up the rounding schedule and technology for virtual family-centred rounds. Your specific tasks include:
For more information about these responsibilities, please view the resources below: |

Training for Physician team members and Learners
Find more information on the roles and responsibilities for Physician team members |
|
This training is for all members of the physician team, including: attending Staff physicians, residents, physician extenders (ie. Nurse practitioners, physician assistants, etc.) medical students. This information applies to the core most responsible physician (MRP) team rounding on each patient daily. If you are a consultant physician please refer to the “Health professionals and Consulting Physicians” section below. As a member of the Physician Team, you are responsible for starting rounds on time, leading a focused rounds discussion and coordinating with the inpatient units to ensure rounds run smoothly and everyone has an opportunity to participate if they wish. For more details about physician team roles and responsibilities, please view the training video and resources below: |

Training for Health-Care Professionals and Consulting Physicians
Find more information on the roles and responsibilities for Health-Care Professionals and Consulting Physicians |
|
This includes, pharmacists, social work, dietitian, respiratory therapists, physiotherapists, occupational therapists etc. As a Pharmacists or other Health Care Professionals (HCPs), you are invited to join rounds as appropriate. Your participation is highly valued during rounds so that the entire multidisciplinary care team — along with the patient and/or caregiver — can make decisions together. Your involvement is embedded in the CHEO rounds standard content above. At CHEO there is a schedule and process supporting routine participation of the on-service clinical pharmacist on rounds. Pharmacists access the videoconference meeting IDs using a shared email/calendar. The pharmacist(s) on service will join rounds for one or more teams based on the pharmacist rounding schedule and are available for consult as needed if not present on rounds. Other Health Care Professionals and consulting physicians are encouraged to participate in rounds for patients they follow. Please connect with unit clerks to obtain the vFCR rounding schedule and videoconference information required to join at the appropriate time. |

Training for Administrative Assistants
Find more information on roles and responsibilities for Administrative Assistants |
|
Administrative assistants have the important responsibility of scheduling virtual family-centred rounds on behalf of the multidisciplinary care team. Specifically, your tasks include:
|

Implementation Considerations
Learn more about vFCR implementation considerations |
||||||||||||
|
There is a body of literature highlighting the benefits and challenges experienced by organizations implementing family-centred rounds. Successful implementation processes will vary, but here we provide general recommendations and examples of how each impacted implementation at our own hospital. We gratefully acknowledge the team at the University of Wisconsin for their work and sharing of implementation principles for family-centred rounds.
|
Technology Considerations
Learn more about vFCR technology |
||||||||
|
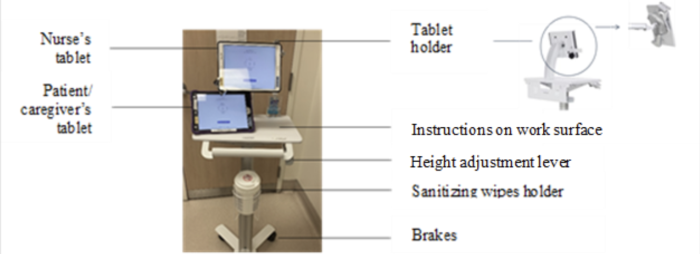
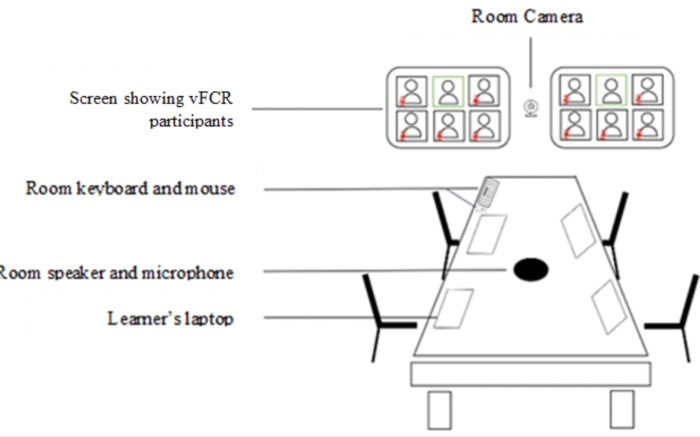
There is a wide selection of consumer (ie. commercially available) products and healthcare grade products available to support inpatient virtual care workflows. We conducted user requirements evaluation and usability testing to support selection of appropriate end user devices. Our device setup was initially based on readily available products (i.e. what we had on hand) which was later optimized once external project funding became available. In our experience, using consumer products with familiar interaction mechanisms and user interfaces supported faster implementation and reduced the need for extensive training.
|
More information about this Toolkit
Our team |
Co-Principal Investigators
Co-Investigators
Research Staff
Collaborators
|
Acknowledgements |
|
We gratefully acknowledge the support of CHEO’s Executive Leadership Team, Incident Management Team and eHealth Leadership Team for their support in this work. We also recognize our project team for their invaluable contributions and hard work in the success of this project – Kerry-Lynne Hall, Helen Yoxon, Melissa Michaud, Chantal Nolet, Angel Boyer, Laura Strachan, Leanne Finlay and Keith McIntosh. We are also grateful for the enthusiasm, patience and support of our patient-facing health-care providers. We gratefully acknowledge the following for their feedback and contributions to this toolkit:
|
Funding |
|
This project was funded by the Children’s Hospital Academic Medical Organization (CHAMO), Innovation Fund 2021-2022. |
Publications and media |
|
How to reference this Toolkit |
We suggest using the following citation for this toolkitBuba M, Dulude C, Et. Al. ."Virtual Family-Centred Rounds (vFCR) Toolkit: An Implementation Guide for Health-care Leaders and Providers. Ottawa, ON: CHEO; 2022. Available at: https://www.cheo.on.ca/en/vfcr-toolkit The details of the methodology and findings from the evaluation study of virtual rounds at CHEO, which was used in the development of this toolkit are available in the following article: Coming soon If you use these materials, we ask that you please cite the above article as well as this toolkit. |
Questions or feedback?
We're here to answer questions and look forward to your feedback to help improve our Toolkit. Please email Dr. Melanie Buba or Catherine Dulude.
How to print this Toolkit
For best results make sure background graphics are enabled.