For best results make sure background graphics are enabled.
What is a febrile (fever) seizure?
A febrile seizure is a seizure (convulsion) that happens while a child has a fever. A fever is a temperature greater than 38°C (100.4°F).
Who gets febrile seizures?
Febrile seizures:
- Are the most common type of seizure in children.
- Happen most often in children between the ages of 6 months and 5 years.
- Often run in families, so other people in the family may have had them as children.
What does a seizure look like?
Febrile seizures are usually brief and only last a couple of minutes.
A child having a febrile seizure:
- Will have sudden, uncontrolled movements or stiffening of the arms and legs
- Will have eyes rolling back
- Loses consciousness during the seizure
- May have noisy breathing
- Will wake up when the movements stop, but may be sleepy for up to an hour after.
Do febrile seizures cause any harm?
No. Febrile seizures have no serious or lasting effects. Children who have had febrile seizures develop and learn at the same rate as other children.
Does a febrile seizure mean my child has epilepsy?
Most children who have a febrile seizure do not have epilepsy. Studies show that 97% of all children who get febrile seizures do not have epilepsy later on. Most children outgrow febrile seizures by the age of 5 years.
Will my child have seizures with every fever?
No. Most children only ever have one febrile seizure in their lives. There is a 1 in 3 chance that your child will have another seizure with a fever in the future.
What should I do if my child has another seizure?
- Stay calm. In most cases, the seizure will stop on its own within a couple of minutes.
- Stay with your child. Don’t leave your child alone.
- Lay your child on a flat surface. Turn your child onto their side. If your child is vomiting, turn them face down towards the floor.
- Do not put anything into your child’s mouth.
- Do not put your child in a bath to try to lower the fever during a seizure. If your child is in the tub when a seizure starts, take them out right away.
- After the seizure, take your child’s temperature to check if there is a fever.
- Observe your child during the seizure so you can tell the doctor:
- where the seizure started (arm, leg, face, etc.)
- what parts of the body were involved (just one side or all over?)
- wow long the seizure lasted
- how your child acted when the seizure was over and how long it took until they returned to normal
Call 911 if the seizure lasts more than 5 minutes.
You’ll need to come back to the emergency department if your child:
- Has another seizure.
- Is very irritable or sleepy and doesn’t improve with fever medicine.
- Has trouble breathing.
- Has signs of dehydration like dry mouth, or is not passing urine (peeing) at least every 8 hours.
- Has a headache or sore neck that does not go away with fever or pain medicine.
You’ll need to see your family doctor if your child:
- Has a fever for more than 5 days.
- Is not getting better after 1 week of symptoms.
- Develops an ear ache.
Fever medicines
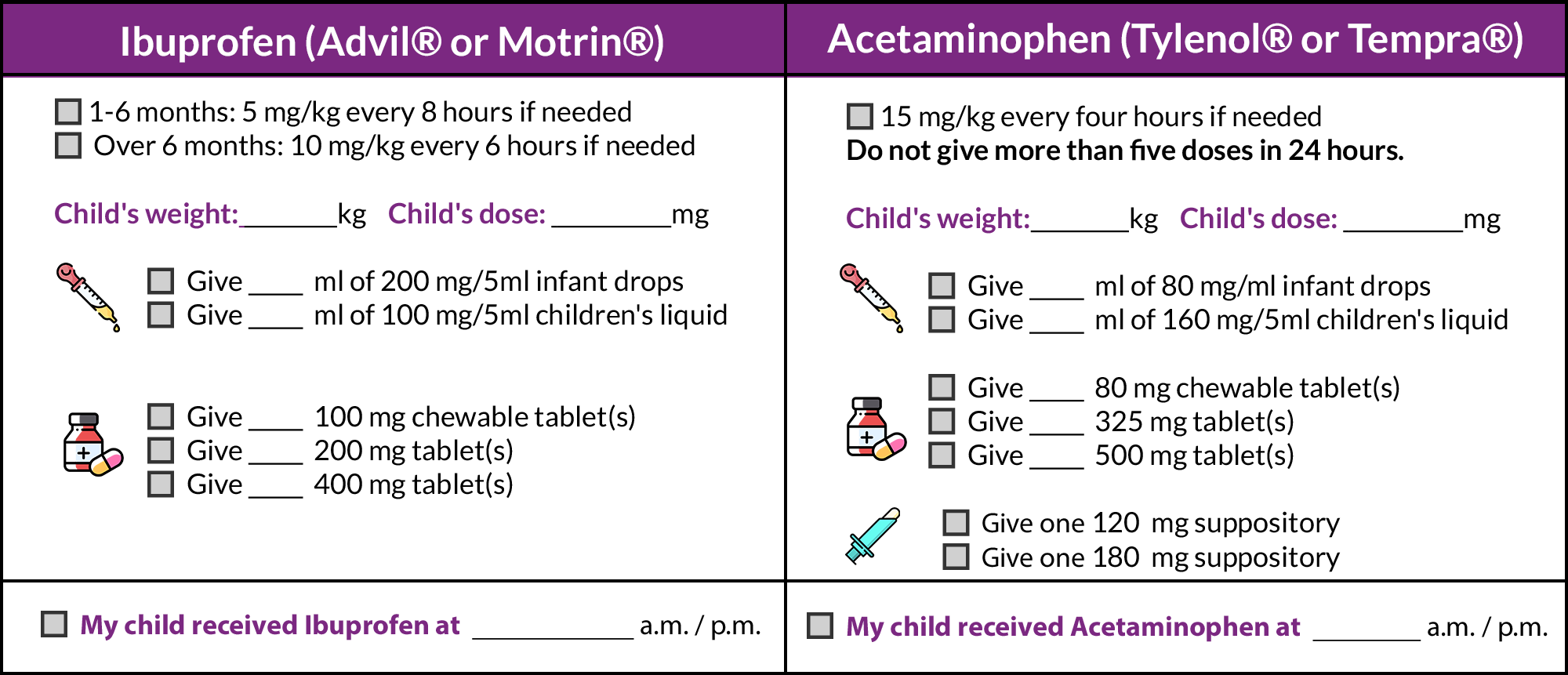
Ibuprofen and acetaminophen can make your child more comfortable by bringing down the fever a little. Most children will not need to have both of these medications.
When your child has a fever:
- Try ibuprofen first, as it works better for most children. Use acetaminophen instead of ibuprofen if your child has a fever due to chicken pox.
- Try acetaminophen if your child does not improve one hour after taking ibuprofen
- Do not use Aspirin® (ASA).
How much should you give?
Medicines for fever and pain come in different concentrations (the number of mg of medicine in each mL, tablet or suppository). Check the concentration on the bottle, and read the package directions carefully. Make sure that you give the dose based on your child’s weight, not age.