Congratulations on the birth of your baby!
While this is a happy time, we understand that a hospital stay can add a lot of stress and can be a scary time for you and your family. We’re here to help you through it and provide you with what you need to know about your baby’s stay in our Neonatal Intensive Care Unit.
At CHEO we have a level 3 NICU. This means that we provide the highest level of care for babies born at the youngest gestational ages to those at full-term. Your baby is here to receive neonatal intensive care which can include breathing (ventilatory) support and specialty services from one or more of our specialty medical or surgical teams at CHEO.
Congratulations on the birth of your baby!
While this is a happy time, we understand that a hospital stay can add a lot of stress and can be a scary time for you and your family. We’re here to help you through it and provide you with what you need to know about your baby’s stay in our Neonatal Intensive Care Unit.
At CHEO we have a level 3 NICU. This means that we provide the highest level of care for babies born at the youngest gestational ages to those at full-term. Your baby is here to receive neonatal intensive care which can include breathing (ventilatory) support and specialty services from one or more of our specialty medical or surgical teams at CHEO.
Transport to the NICU |
||||||||||
| By this point you have likely met the friendly faces of our Transport Team. They travel with their fully functional portable NICU which has everything your baby needs to make it safely to CHEO. Their isolette is heated and your baby is secured in a 5-point harness. Their equipment allows for transport of the most complex NICU patients and our team is specially trained to care for them en route. Members of the team are usually a registered nurse or respiratory therapist who are trained in both roles, called a transport clinician. They are always only a phone call away and in constant communication with the neonatologist (specialized newborn doctor) who approves and recommends the treatments your baby needs. There may not be room in the ambulance or plane for a parent to accompany their baby, but we do our best to accommodate this when possible. |
||||||||||
Unit setup |
||||||||||
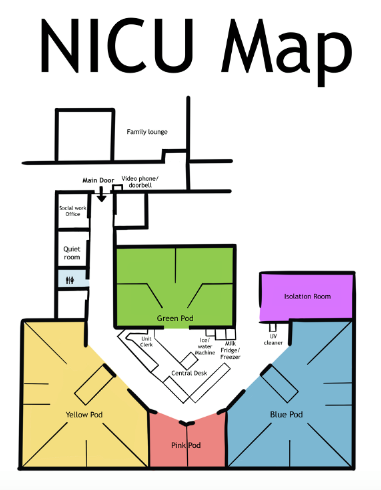
| We have three main rooms, which we call “pods” that are identified by colours – yellow, blue and green. There are two rooms near the central desk that make up the “pink pod” The colours do not represent anything other than the location of your baby. Babies of any degree of illness can be in any pod. There are times when we have to move babies from one pod to the other to balance out numbers and keep the workload even for our nurses. There is a screen located next to the unit clerk’s desk where you can see the location of your baby and the name of the nurse assigned for that shift. If your baby has moved location within the unit, this will always be up to date. Your baby will never be moved outside of the unit without notifying you first.
|
||||||||||
Parental presence in the NICU |
||||||||||
Parent, caregiver and visitor presence policiesPlease review the following information before arriving at CHEO. Parents and caregivers are important members of the care team. They actively work with us to provide vital health information only they know and give emotional support in the way only a parent or caregiver can. For infection prevention and safety reasons, we have limits on how many parents, caregivers and visitors can be onsite at one time. We also limit the number at the bedside. We appreciate your patience and understanding in keeping everyone safe, particularly during the peak viral season. Allowed number of parents, caregivers and visitorsLast updated: December 2025
Frequently asked questions about coming to CHEO
|
||||||||||
Access cards and safety |
||||||||||
| For your baby's safety, the NICU is a locked unit. Once you visit the Admitting Office, located near the main entrance, you will be identified as a parent and will receive one unit access pass per family. There is a deposit fee for the pass card which you will be refunded at the end of your stay. Once you have your access pass, you can swipe yourself in and out of the unit. If you do not yet have an access pass, there is a video phone and doorbell at the NICU doors that you can use for staff to let you in. For everyone’s safety, please do not share your pass with anyone else. |
||||||||||
Getting information about your baby |
||||||||||
| You can call the unit at any time for an update on your baby. When you identify yourself as a parent, ask to talk to your baby’s nurse to receive an update. There may be times when your baby’s nurse is busy caring for your baby or busy at shift change (around 7:30 both in the morning and in the evening) when they cannot come to the phone. In that case we’ll arrange a call back at a more appropriate time. |
||||||||||
Handwashing and safety |
||||||||||
| Babies in our unit are at high risk for infections and hand washing is one of the best ways to keep them safe. Start by removing your outside jacket (if applicable) and store it in the shelving unit in the corner of your baby’s room, this is your space. Next, remove all rings, watches, bracelets and any jewelry below the elbows. Please give a good scrub to your hands, being sure to get beneath the nails, between each finger, and the backs of the hands. Dry thoroughly with the paper towel provided. Hand washing videos: |
||||||||||
Cell phones in the unit |
||||||||||
| You are able to use your cell phone while in the unit. There is a UV cleaner that we recommend you use to sanitize your phone, especially when you first arrive in the unit and before you head into your baby’s room. It is expected that you use your cell phone for personal use only. You may not take photos or videos of other families or babies without expressed consent. If you are speaking on the phone, please remember to use a quiet speaking voice or leave the room for your call. As a courtesy to everyone in the room, please use earphones when listening to audio or on a video call. Please keep ringtones and alerts on silent mode. iPadsIf you cannot physically be in the unit due to distance, illness or other circumstances, we can connect with you via teleconference for a brief visit with your baby or to join in daily rounds with the NICU team. |
||||||||||
Room setup |
||||||||||
| Each room is set up with a bed most appropriate for your baby. This can be a heated overbed, an isolette or a cot. Sometimes there is a lot of equipment setup on all sides of your baby’s bed, depending on their needs. You may use the pull-out bedchair or the rocking chair. The cupboards in the corner are for you to store your jacket, purse and other personal items. Some parents choose to wear indoor shoes while in the unit or bring linens for their baby and store them here. You’re welcome to bring a photo or a drawing from a sibling to personalize the space. Some choose to bring books to read to their baby and store them here. We can provide a breast milk pump for this corner, and there is a white light switch that is dimmable for you to access an overhead pot light. |
||||||||||
Meals |
||||||||||
| In the Ronald MacDonald family lounge across the hall, there is a small kitchenette where you can store meals and heat up with a microwave. Be sure to mark food with your name. There is a second family lounge located on the 5th floor (5 West). You are welcome to have a small snack or drink from a covered beverage at the bedside, however larger or smell-producing meals are to be kept outside of the unit. You’re welcome to eat your meal in the family lounge, at one of the many picnic tables outside or at the Rainbow Café seating on the 1st floor. Visit CHEO’s Amenity page for more information. Staying at CHEO? Order food to your bedside.CHEO patients, parents and caregivers can now place an online order for food right to the bedside, using the CBORD® Patient™ app! Click here for more information, and to download the app. |
||||||||||
Accommodations |
||||||||||
| There is a pull-out bed chair at each baby’s bedside where one parent can stay the night. The NICU and PICU share a few parent sleep rooms located in the Ronald McDonald Family Lounge. These sleep rooms are reserved for parents arriving from out of town at night or parents whose child is extremely sick or awaiting surgery in the morning and want to remain in hospital. They are intended for short-term accommodation. Visit CHEO’s Amenities page for information about Ronald McDonald House and Rotel which are located next to the hospital. |
||||||||||
Parking |
||||||||||
| Parking is available on-site. To purchase a parking pass, visit the security office, located on the 2nd floor near the emergency department. Many parking pass options are available and our Security team can help you find the most economical option. | ||||||||||
Unit map |
||||||||||
| The NICU is located on the 3rd level. The main entrance is located on the 2nd level of CHEO. Visit our Maps and Locations page to see maps of each floor at CHEO. |

Your baby's stay in the NICU
Who's who in the NICU |
||||||||||||||||||||||||||||||
|
You will meet many new faces throughout your stay in the NICU. It takes a large team to cover all the needs of the babies in our unit.
|
||||||||||||||||||||||||||||||
Monitors and alarms |
||||||||||||||||||||||||||||||
|
One of the first things you will notice is that we attach many wires to your baby. The three stickers on their chest and abdomen will monitor their heart rate and breathing rate. The glowing red light on their hand or foot measures their oxygen saturation. These alarms are very sensitive and will sometimes ring unnecessarily when your baby is moving or the wires are not in a good position. Nurses are trained to know very quickly when these alarms require immediate action and when it is a false alarm. If you are worried, always look at your baby for reassurance of how they are doing. What do those numbers mean?
|
||||||||||||||||||||||||||||||
Specialty services available |
||||||||||||||||||||||||||||||
| At CHEO we have specialist doctors and teams for almost every system in your baby’s body. Specialty services will be consulted only when they are needed. These include teams such as General Surgery, Cardiology, Respirology, Genetics, Neurology, Ear/Nose/Throat (ENT), Nephrology, Opthamologists, Anesthesia, Pain and Symptom Management, Feeding (occupational therapy) or physiotherapy and many more. All of these specialists act as a consultant while your baby is still under the primary care of a Neonatologist. | ||||||||||||||||||||||||||||||
Home criteria |
||||||||||||||||||||||||||||||
|
All babies have the same basic criteria to go home:
With all of those goals met your baby is set to go home! BreathingMany of the babies in our unit have breathing difficulties at birth. Once these issues are resolved, they sometimes still have “spells” or short pauses in their breathing.This is most common with premature babies and it causes their heart rate and oxygen saturations to drop. As the respiratory center in your baby’s brain develops this will stop happening. Your baby will eventually breathe consistently even while in a deep sleep. We require babies to be spell-free for seven days prior to discharge to be sure they will not do this at home. FeedingMost babies do not start to coordinate their suck, swallow and breathing pattern until somewhere between 32-34 weeks gestational age. Many of the babies in our unit have additional issues as they may not start eating by mouth until later than this. Your baby needs to be breast or bottle feeding reliably before they go home. If it is determined that feeding issues may last a long time, we may set up tube feedings and equipment for home. With the first two criteria met, the last piece that lets us know your baby is ready for home is weight gain. Weight is monitored every day. If weight gain is not a concern, we may space it out to once or twice a week. Maintaining temperatureFor premature babies who have been in an isolette or overbed warmer, we need to make sure they are big enough to maintain their temperature. If they spend too much energy trying to keep warm, they will not grow well and may tire out more easily. In an open cot with normal clothing and bundling, your baby should be able to maintain a normal range temperature before going home. Parent learningSome babies will have specialized needs for home. All follow up appointments, home medications, and home equipment needs will be arranged before you are discharged home. We will make sure you know what appointments you need to attend, how to give and obtain any medications your baby requires, and are comfortable using and adequately supplied with any medical equipment they may need at home. Some conditions require further parent teaching and we need to be sure you have received any education you need to safely bring your baby home. Hearing ScreenAll babies in Ontario receive a hearing screen within the first two months of life. We try to get this done while your baby is in hospital. If your baby is discharged before it is done we can arrange for the screen to be done in the community. |

How to get involved in your baby's care
Learn the language of the NICU |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Click through our glossary to learn more about the terms and phrases you might hear your baby's care team using. You can click on the letters below to jump to the words starting with each letter.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Daily rounds |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Every day our NICU Team meets for their daily rounds. Rounds start at 9:30 but it takes a few hours to get around to each patient. The team reviews your baby’s condition over the last 24 hours and makes a plan for the next 24 hours. There is sometimes open discussion or teaching for residents included and a lot of medical terms being said. The team will make sure that you understand all of the important pieces of what was said and give you an opportunity to ask questions. Some parents find it helpful to write down their questions so they don’t forget them when the whole team is there to ask. If a lengthier discussion is needed on a certain topic, sometimes we need to prioritize and come back later to discuss details. We can arrange to have you attend rounds by secure video conference or fill you in on discussions later in the day if you cannot be there in person. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Handling times |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Because sleep is so important for your baby’s development, we try our best to set a schedule for your baby’s care or “handling” to minimize disruptions. If your baby is being fed, all of their care is then clustered around their feeding times. Often these times are every three hours and either start from 8am or 9am and continue around the clock every 3 hours. If your baby is not being fed, we may aim to provide care every 4 hours. There may be occasions we will adjust these times to coordinate with a test that needs to be done or based on your baby’s cues. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Interacting with your baby |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Sometimes the tubes and wires can be scary and overwhelming. Your baby is still there behind all of it and there are many things you can do to care for them. You can talk or sing to your baby in a quiet voice, but sometimes it is hard to know what to say to your baby. For these times, we are lucky to have books donated to the unit as a special gift from the family of Jack & Mia. You can read this book that is given to your family or any other book you choose to bring in. You can also hold their hand or show them a small toy. If they are well enough you may be able to try supervised tummy time to help strengthen their back and neck muscles. You can always get involved in your baby’s care by taking their temperature and washing their face or cleaning their mouth and eyes when needed. You may need some help with the wires at first, but you can help change your baby’s diaper around the time of their feed or handling time. Family members who cannot visit in-person may want to spend time with the baby by video call. We kindly ask that you use earphones and a quiet voice to respect the space of the other babies in the unit. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Bathing and care |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
When your baby first arrives in the NICU, they usually have several tests or procedures, consults, or exams from physicians which makes daytime quite busy. We also like to give you time to cuddle your baby during the day. This means that we usually reserve bath time for the night shift as there is more available time. Weights tend to be done at the same time as the bath and on Saturday nights we take all of your baby’s weekly measurements (height and head circumference). As your baby gets better and is moving closer to home, days become less busy with tests and procedures. At this point we encourage parents and caregivers to be more involved in daily care and we can teach you how to bathe your baby during the day or evening if you prefer. While this routine usually works well, let us know early if there is another arrangement that we can try to accommodate. With your baby’s handling times, you’re welcome to provide care such as eye and mouth care when needed and a diaper change. The nurses will help you navigate all of the equipment and wires. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Feeding, supports and pumps |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
It is common in the NICU that babies are not ready to feed by mouth for the first while for various reasons depending on their condition. In this case, your baby will receive all of the nutrition they need via an IV. This total parenteral nutrition is called TPN and is made up of sugar, electrolytes, vitamins and the fats your baby needs to grow. It is made especially for your baby based on their blood values. If your baby is ready to receive small amounts of breast milk or formula, this will be offered by a nasogastric tube (NG). The NG tube is inserted in their nose or mouth, travels down their esophagus to their stomach and can deliver milk. If your baby has no issues breathing and is showing signs that they are ready to bottle, breastfeed or chestfeed, they will be allowed to try feeding by mouth. Sometimes it takes a few tries for them to learn how to feed by mouth and build enough energy to get through an entire feed. We often use a feeding tube to give any remaining milk they were unable to take by mouth. All of our nurses have extensive training and experience helping mothers with breastfeeding or chestfeeding. From day one we will get you set up with a breast pump and all the information you need to know about pumping. We have pumps available at the bedside and will provide you with one breast pump kit for your stay. It is your responsibility to care for the kit and safely store your milk. If possible, we would like to use fresh milk to feed your baby. Any milk not being used within one hour after pumping needs to be kept cold in the refrigerator or on ice and labeled with the date and time you pumped. Our pumps cannot be removed from the hospital. If you choose to go home overnight and need to pump, you may need to purchase or rent a pump for home. We can instruct you where to find a rental pump. In the meantime, you can always use hand expression to help keep your supply up and for comfort. Expressed breast milk (EBM) can be stored:
Once thawed out, it is good for 24 hours. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Kangaroo care |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
As much as possible, we encourage all parents to provide kangaroo care which involves uninterrupted time for either parent to hold your baby skin to skin. Your baby will be in just a diaper and rest on your bare chest. We recommend that you make sure you’ve had something to eat and drink and gone to the bathroom prior to holding your baby. This will help make sure you are available for at least 60 minutes but kangaroo care can last several hours if you’re able. It can take some time after transferring to your skin before your baby really settles in and it is best to minimize disruption. This time is so precious with your baby and we advise you to soak it all in and not pick up your phone and maintain skin to skin contact with your baby for as long as possible. Benefit of Kangaroo Care for babiesSkin-to-skin or kangaroo care has been shown to have many benefits for your baby. It helps them:
Studies show when you and your baby are skin to skin in the same environment, you produce antibodies to microorganisms in this environment which. These antibodies appear in your breast milk within a few hours and the immunity is passed on to your baby. It also is shown to help with sleep and brain development Benefits of Kangaroo Care for parents:
Modified Kangaroo CareIf your baby’s condition prevents them from being held, there are modified forms of kangaroo care you can provide.
More information |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Linens and clothes |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| You may choose to bring in some blankets, facecloths, or clothes for your baby. Make sure items are washed in a scent-free detergent prior to bringing them in. Your home should be smoke-free before your baby’s arrival as the scent of smoke can cause them difficulty breathing. Make sure your items are labeled with their name (usually on a tag). While we try our best to keep things clean, babies are messy beings. Blankets will frequently be soiled and have to be brought home to be laundered. Just in case, do not bring items that are very precious to you or you would not like to be lost or accidentally damaged. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Bravery beads |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Your journey in the NICU with your baby is unique. Thanks to the CHEO Foundation, we have created a bravery beads program. In the parent area of the NICU you will find colourful beads that each have a special meaning. You can create a representation of your baby’s journey in the NICU by collecting a special bead for each test, procedure or occasion they go through. Each one has a meaning and this collection you create will be a testament to their story for years to come. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Transition to pediatric care |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
As your baby’s health improves, they may not need NICU care any longer. If they are not requiring the specialty care of our NICU, there are times when it is appropriate to send them back to their birth hospital or transition to another unit at CHEO before they’re ready for home. While the care may look different in different areas, know that this is a positive move towards the goal of you bringing your baby home. This will give you the opportunity to become even more involved in your baby’s everyday care. What you can do to ease this transition?Get involved in your baby’s care early on. While you are in the NICU, try to learn as much as you can to become the expert in your baby’s care. If your next step is the inpatient wards at CHEO, parents are expected to stay with their baby. Most parents who have had their baby home already want to stay and are used to caring for their child. This parent-led care model can be a big change for parents of babies who have been in the NICU but this is progress towards going home! Learning how to lead your baby’s care early on will help. Ask for help! Child Life is there to improve your child’s experience. They can help coordinate volunteers to cuddle your baby when you need a break. Social Workers are there to support you and help you navigate the health care system. Spiritual Support are there to listen and help you through difficult times. Patient Experience is there to respond to questions or concerns you may have about your time at the hospital. |

Feeding in the NICU
Most babies who need to come to the NICU may not be able to feed as they normally would for the first few days or longer. For various reasons, both term and premature babies may have issues with breathing or digestion that prevent them from feeding. Initially, they will receive all of the sugars and electrolytes they need by intravenous (IV) fluids.
If you plan to breastfeed, chestfeed, or provide your baby with expressed breast milk, you should start expressing milk as soon as possible. In the first few days your milk is darker and thicker, called colostrum. Save every drop! We call it Liquid Gold and it contains many protective factors to line your baby’s digestive tract. Even if your baby isn’t ready to feed, we can put a small drop in their mouth which we call Oral Immune Therapy (OIT). It helps get your baby’s bowel started on the right track.
IV feeding (TPN) |
|
If it is determined that your baby cannot eat for more than a few days, we will add in extra nutrition that includes all of the vitamins, proteins and fats they need to grow and thrive. This intravenous (IV) nutrition is called Total Parenteral Nutrition or TPN. Your baby’s TPN is prepared every day and adjusted to your baby’s specific nutrition needs based on their blood values. They will have regular blood work drawn to make sure they’re getting the right amount of everything they need. We will often make adjustments in the rate of TPN as we try giving your baby more of your milk by mouth or through a feeding tube. |
Tube vs bottle feeding |
|
When a baby is ready to start receiving milk, there may be several reasons why we need to start with a tube or bottle feed. Premature babies start to develop a stronger suck and coordinate with their swallow around 32-34 weeks gestational age. Some full term babies may not be able to feed by mouth if they have breathing, neurological, digestive or other issues. If your baby’s breathing or suck prevents them from being able to take their feed by mouth, we will insert a nasogastric (NG) tube in their nose that will deliver the food directly to their stomach. This allows your baby to safely receive milk without the risk of choking (aspiration). Tube feeding allows them to save their energy for growth and development. After not feeding for some time, your baby will start with a small amount of breast milk or formula. This small amount of milk that is meant to get your baby’s digestive tract used to the idea of feeding is called a trophic feed. When your baby is tolerating trophic feeds we will slowly increase the amount of milk they receive. |
Breastfeeding or chestfeeding in the NICU |
|
Your human milk is designed to give your baby everything they need. Mothers of premature babies produce milk with a different makeup than those of full term babies. It has more calories and a different nutritional makeup that changes as your baby grows. When your baby is old enough and healthy to feed on their own, they will begin showing signs of readiness to feed. Opening their mouth, rooting and showing a strong suck are all some of the signs they’re ready to start feeding. Even for full-term, healthy babies this sometimes takes a bit of practice, patience and learning for both mother and baby. Your baby’s nurse can share tips to help you succeed. For more information on breastfeeding or chestfeeding, please visit our CHEO breastfeeding and chestfeeding resource page |
Pumping in the NICU |
|
For parents who are choosing to breastfeed, expressed milk is the best gift you can give your baby until they are ready to go to the breast. It contains so many nutrients and protective properties for their bowel and immune system. It’s no secret that expressing your milk is a lot of work. Even if only for the first few feeds, mother’s milk is proven to provide your baby with lifelong benefits. We have a double pump for you to use, available at your baby’s bedside. We provide you with one kit that you will be responsible for caring for throughout your stay in the NICU. There is also a lactation room in the Ronald McDonald Family Lounge where you can find a dishwasher to sterilize your kit once a day. In between you will be provided with a bowl and dish soap to wash and air dry your kit at the bedside. After delivery, the hormone prolactin which helps you produce milk increases. You need to stimulate the breast tissue to encourage milk production. Early breast massage or hand expressing is the best and easiest way to remove this early milk called colostrum. We encourage you to express your milk every 2-3 hours. It may be helpful to set an alarm to keep you on track. During the first few days or weeks it will be necessary to pump through the night as prolactin levels are highest between 02:00-04:00 in the morning. You can find more information on pumping and milk production here. We recognize that it is a balancing act between sleep, nutrition, your pumping schedule and all of your demands. While you may have never considered pumping when you envisioned taking care of your newborn, keep in mind it is hopefully one step towards breastfeeding or chestfeeding your baby one day soon. A Pumping log that may be helpful for you to track the times and amount you pump each session. You may be able to notice trends such as whether your supply increases or decreases based on stress, nutrition, when you spend time near your baby or frequency of pumping. |
Hand expression |
|
There are many advantages to expressing milk by hand and it may even be the best way to express colostrum during the early days. Colostrum is particularly thick, rich and nutritious for your baby, but the thick milk can be difficult to extract using an electric pump. Hand expression really helps you get deep into the tissues to help stimulate production and clear the ducts. Here is a short video from BC Women's Hospital that explains the technique. |
Baby led feeding cues |
|
To know when your baby is ready to feed, we will look for cues they are ready to feed. When the medical team has cleared your baby to feed, we will look for signs they are ready to feed such as sucking, rooting or opening their mouth, licking, or bringing their hands to their mouth. If your baby is sleepy, there are some ways of gently waking them. It might be necessary to try timing feeds with moments when they are already awake and keen to feed. With time, they will feel more hungry and be keen to feed. If your baby is not feeding by mouth yet, it is important to create positive oral experiences for them. Providing opportunities for non-nutritive sucking such as a pacifier or soother, allowing them to nuzzle at the breast, or sucking on a clean, upside down finger in their mouth to soothe all help create a positive oral experience for your baby. You can also gently stroke their cheek and speak to them when they are happy. Providing a drop of breast milk on their tongue, called Oral Immune Therapy and may be a positive oral experience that also allows them to smell and taste your breast milk while also providing them with antibodies from your milk. |
Monitoring growth |
|
Whichever type of nutrition your baby is receiving, their growth will be closely monitored. We measure their weight daily if possible. The doctors, dietician and nurses will make adjustments to their feed if needed. Premature babies or those with a cardiac condition may require extra calories or nutrients added to their milk. Sometimes babies require additional nutrition to grow and thrive. There are two types of fortifiers that could be added to your breastmilk; one is made from cow’s milk and the other is made from human milk. Be sure to speak to your baby’s neonatologist and dietitian to understand all of the options and what is best for your baby. You can find more information on breastmilk fortifiers from PreemieWorld here. |
Donor milk |
|
Some babies who are born very premature or with certain gastrointestinal (GI) issues may qualify to receive Pasteurized human donor milk (PHDM). There are strict criteria for those who qualify to donate and all milk is collected under strict conditions and stored in a human milk bank. It is then pasteurized to remove any potential germs, yet still contains all of the benefits of breastmilk. This is a similar process that happens with cow’s milk that you buy in the grocery store. We do not allow for milk sharing or wet nursing in the NICU. If you have excess milk supply and are interested in donating breastmilk for premature and critically ill infants in our province, you can find out more information on Milk Bank Ontario's website. |

Neonatal Encephalopathy (HIE and cooling)
Please see the selection of helpful information that may be relevant to your stay in NICU or useful for when you’re at home with your baby,
What is Neonatal Encephalopathy (HIE and cooling)? |
| It is a general term that means swelling or injury in the newborn brain that disturbs its function. There are many ways this can happen before, during or shortly after a baby is born. Hypoxic Ischemic Encephalopathy (HIE) is the most common type we see. It is caused by a lack of oxygen at birth can be caused by problems with blood flow from the placenta to the baby. Other causes are neonatal stroke- which is a bleed in an area of the brain- or it can be caused by problems with the baby’s breathing after birth, sometimes due to metabolic issues or an infection in the amniotic fluid. |
How do we treat it? |
|
Some babies with this kind of issue at birth may benefit from therapeutic hypothermia. This is a cooling treatment that lowers the baby’s whole body temperature by a few degrees to slow down brain activity and slow the swelling response. The cooling helps to limit further injury to the brain and helps with recovery.
If you’ve heard the expression “don’t poke the bear” that is because they require a lot of energy to suddenly increase their heart rate, breathing rate and temperature. While babies who are cooling will often wake on their own, it is very important to respect their sleep cycles and allow their developing brain time to heal. |
HIBERNATE in the NICU |
While there are many necessary tests and interventions at this time, it is important to maintain a quiet, calm environment for your baby. There are ways to get involved in your baby’s care. We encourage you to ask your baby’s nurse how you can best provide comfort when they are awake. While it might feel like forever, hibernation only lasts three days and is an important period of healing. |
HIE resources |
|
The following websites explains much of what you can expect during your NICU stay when your baby is cooling and also what you can expect after as they grow and recover: |
Preparing for home
Infant CPR |
|
We want you to be prepared for anything while you’re at home. Make sure you know what to do if your baby were to stop breathing, turn blue or start choking at home. Please watch these videos on infant CPR and talk with your nurse if you have any questions. CPR CPR and choking
|
Infant care resources |
|
Websites Our team has hand-picked the following resources for you:
Factsheets
Videos
|
Parent resources |
Bereavement support |
|





















 To help understand how cooling can help, think of how and why a bear hibernates in the winter. When winter comes, a bear’s food is in short supply. Their body temperature lowers and their breathing and heart rate slow down. By reducing the energy demands on their body, they’re able to go many months without food. As in any injury, after a traumatic birth, the body’s natural reaction is inflammatory to help heal, which causes swelling. By cooling your baby, this limits the amount of swelling, similar to how you could ice an injury. When a baby is cooled, their body’s demands are slowed, in particular in the brain, which helps prevent further injury.
To help understand how cooling can help, think of how and why a bear hibernates in the winter. When winter comes, a bear’s food is in short supply. Their body temperature lowers and their breathing and heart rate slow down. By reducing the energy demands on their body, they’re able to go many months without food. As in any injury, after a traumatic birth, the body’s natural reaction is inflammatory to help heal, which causes swelling. By cooling your baby, this limits the amount of swelling, similar to how you could ice an injury. When a baby is cooled, their body’s demands are slowed, in particular in the brain, which helps prevent further injury.